
Is Chorus Right for You?
Are you constantly battling stomach issues and wondering if an herbal supplement could help? Chorus might be what you need, but it’s not for everyone. Let me ask you some questions and see if Chorus is right for you.

Do I Have Digestive Problems?
Sometimes it’s obvious you have digestive problems, and sometimes it’s a bit more subtle.
So, there are two things that you need to ask yourself.

1. What Does My Tongue Look Like?
This question looks at the start of your digestive system.

2. What are my Poops like?
This question looks at the end of your digestive system
What Does My Tongue Look Like?
There are many subtleties in examining tongues, but when in doubt, compare your tongue with that of a friend who doesn’t have stomach problems and see if they look similar. If they don’t, you might need to work on your digestion.

First, look at your tongue. If you have a thick tongue coating, Chorus might be right for you.
To see if you have a thick tongue coating, look for a dense, white or yellowish layer covering your tongue. This coating usually feels pasty or furry and is more noticeable toward the back. A healthy tongue should appear smooth and mostly pink.
What Are My Poops Like?
Next, consider your bowel movements. If they occur regularly-usually once a day and are well-formed, you’re doing pretty well.
How often?
Likewise, an unhealthy bowel pattern might include going more than three times a day or less than three times a week. If your bowel habits fall outside these norms without a clear, temporary cause, Chorus could help you.

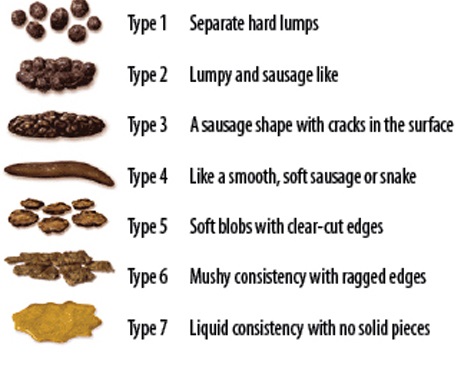
What is the Consistency?
Unhealthy bowel movements can vary significantly: they may be too hard or too soft, occur too frequently, or not often enough. If you consistently experience stools that are hard and difficult to pass or loose and watery, these could be signs of digestive issues.
Do I have any other Indicators of an Unhealthy Gut?

How is Your Stomach?
We skipped over the stomach and small intestine, but if you have excess burping, GERD, cramping, or excessive gas, these are signs of an unhealthy micorbiome.
How Long Does it Take?
If it takes you a really long time to poop or if you have sudden urgency, these are indicators as well of a unhealthy microbiome.
Is My Digestion Affecting My Health?
To determine if your stomach issues are impacting other aspects of your health, you can conduct a simple self-test over two weeks. Focus on three key areas: adjusting your diet, increasing your intake of warm water, and incorporating abdominal massages.
If these things help, then maybe there is a connection between your symptoms and your gut
1. Fix Your Diet.
Try switching things up. What you are doing may not be working so let’s do something different. what you eat can have profound effects on your digestive health and overall well-being. Start by removing foods known to cause inflammation and discomfort, such as gluten, dairy, and excessive sugars.
2. Drink Warm Water.
Drink warm water or tea with ginger, citrus peel, and peppermint. The warm water will help increase motility, and herbs like peppermint can regulate bacteria in your gut.
3. Do Abdominal Massage.
This profoundly simple but powerful technique stimulates the organs and improves blood flow within the abdomen. It can help relax cramped muscles, boost motility, and facilitate regular bowel movements.
How Do You Fix Your Diet?
Inflammatory Foods
If you’re currently not eating well, start by eating better; cut out common inflammatory items like dairy, gluten, and sugar. Most of these types of diets cannot be maintained long-term, but we’re not aiming for longevity here. We are looking at changing your diet for two weeks. We are trying to establish a cheap and easy proof of concept. We want to see if there’s a connection between your gut and your symptoms.
Switch It Up
If you’re already eating well and it's not working, do something different. If you’re fasting, try eating more frequently. If you’re eating all the time, try fasting. If you’re vegetarian, try incorporating more meat; if you’re mainly eating meat, try including more vegetables.
What's Next?
If you follow the above steps for two weeks and start to feel better, then we have confirmed the connection: your unhealthy microbiome is aggravating your other symptoms.
You have three options: antibiotics, which kill bacteria; probiotics, which add bacteria; and supplements like Chorus, which try to balance the bacteria you already have.
When it comes to managing an unhealthy microbiome, relying solely on antibiotics or probiotics often addresses only part of the issue.
1. Antibiotics
Antibiotics can eliminate harmful bacteria and destroy beneficial bacteria, potentially disrupting your gut flora balance further.
2. Probiotics
Probiotics introduce specific bacteria strains, but they may not thrive or integrate effectively if the intestinal environment isn’t supportive. Simply adding more bacteria won’t necessarily address underlying imbalances. To truly benefit from probiotics, it’s crucial to cultivate a healthy gut environment.
3. Chorus
A third option, using supplements like Chorus, offers a more holistic approach. Chorus works to balance and enhance the bacteria you already have, promoting a more natural and sustainable restoration of gut health. This balancing act is crucial as it helps maintain an ecosystem within your gut that can adapt and thrive, ultimately supporting broader digestive health and overall well-being.
When May Chorus Not Be Right For You?
Your digestion worsens with regular movement or exercise
Stomach pain that feels better with heavy pressure.
Stomach pain that worsens after a bowel movement.
You struggle with anorexia or you regularly fast for 48 hours or longer
Shortness of breath
Dizziness upon standing.
Pregnancy or nursing
True Celiac disease (not just gluten sensitivity).
Let Get You Feeling Better Now!
So, if you’re struggling with stomach issues and feel ready for a change, remember that diet and lifestyle adjustments like drinking warm water, practicing abdominal massages, and eating healthier can all help improve your condition.
However, if you’re looking to accelerate your journey towards better digestive health, consider incorporating Chorus into your routine. This herbal supplement balances your microbiome and improves your health. Give Chorus a try and experience the potential benefits for yourself. You’re just a step away from potentially feeling better and living a healthier life!
Brehan Crawford, based in McMinnville, Oregon, is a distinguished clinician specializing in the treatment of chronic conditions, particularly Lyme Disease and its coinfections. After earning his Master’s degree in Acupuncture and Oriental Medicine from the Oregon College of Oriental Medicine in 2009, he deepened his expertise with a 5-year residency under the mentorship of the renowned Dr. Heiner Fruehauf at the Hai Shan Clinic. A Diplomate of Oriental Medicine from the NCCAOM, Brehan has pioneered innovative methods using Traditional Chinese Medicine for chronic infections. Known for mentoring other professionals, he regularly imparts knowledge on advanced Chinese herbal medicine applications. Beyond his clinical pursuits, Brehan enjoys singing, cooking, and hiking.










Recent Comments