
Are Seed Oils Bad?
Ah, seed oils. They’ve become the latest villain in our quest for the perfect diet. As an acupuncturist, I’ve heard countless patients complain about feeling awful after eating out. They often point the finger at seed oils. But are seed oils truly to blame? Or is there more to the story?
The Seed Oil Saga
Seed oils, like sunflower, peanut, and canola oil, have been used for decades. They are a staple in many households and restaurants. Yet, some people claim these oils are the root of all evil. From causing inflammation to chronic diseases, seed oils have been accused of it all.
Downsides of Seed Oils
Upsides of Seed Oils
My Personal Nerd Safari
I was having a hard time reconciling the overwhelming evidence that seed oils are not harmful with the stories of my patients who feel terrible after eating them. So, I went on a nerd safari and found something that I think will help a lot of you.
For context, patients almost always tell me they feel worse after eating at restaurants. And I think that is the culprit is oxidation.
The Culprit Is Oxidation
The hypothesis here is that it isn’t the seed oils themselves that are the problem. It’s the oxidation of those oils. Restaurants often save cooking oil and use it repeatedly. The fastest way to make any kind of oil oxidize is to expose it to light, heat, and oxygen by cooking.
And that’s what a fascinating study in India looked at. They bought some vegetable oil (likely sunflower or peanut oil) and tested it on rats. The rats were fed unheated oil, single-heated oil, and oil that was heated three times. The results were eye-opening.
The Study
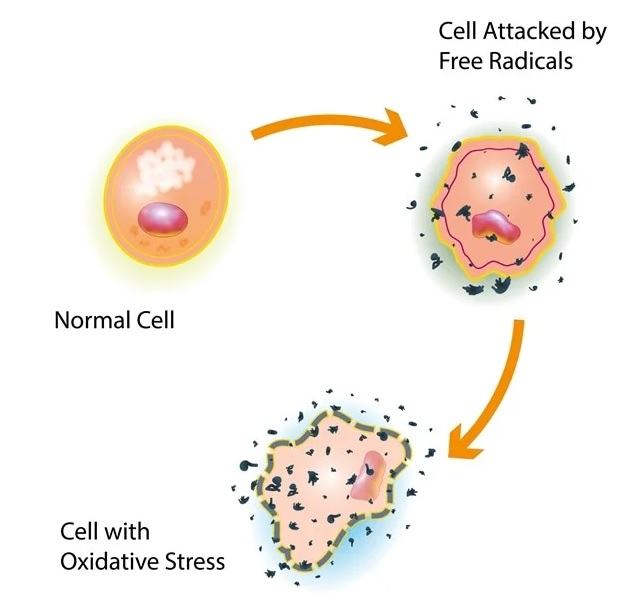
According to the study, repeatedly heating oil increases its oxidative stress. This leads to the formation of reactive oxygen species (ROS), which are harmful compounds known to cause cancer, deplete glutathione, and feed chronic inflammation.
Reactive oxygen species (ROS) are highly reactive molecules derived from oxygen. They include free radicals.Their levels are tightly regulated by antioxidant systems. An imbalance leading to excessive ROS causes oxidative stress, which contributes to aging, cancer, and various diseases
Rats fed triple-heated oil gained more weight, had larger livers and colons, and, most dangerously, developed dramatically more colon polyps. These polyps can turn into cancer. Clinical analysis of blood samples revealed increased levels of glucose, cholesterol, and creatinine in these rats, indicating significant health risks.

What I See in My Clinic
In my clinic, I see patients who feel bloated, sluggish, and generally unwell after dining out. This aligns with the study’s findings. It’s not just the seed oils, but how they are used and abused in cooking that makes a difference.
Tips
- Cook at Home, Use fresh oils and avoid overheating them.
- If you must eat fried foods, try to consume them early in the day when the oil is likely to be fresher.
- Use seed oils in moderation and balance with sources of omega-3s like fatty fish, walnuts, and chia seeds.
- Consider using less refined seed oil options like high-oleic sunflower or safflower oil over highly processed varieties.
- Incorporate a variety of minimally processed plant oils like olive, avocado, and nut oils into your diet for a healthier balance of fats.
- Incorporating herbal supplement Chorus into your routine. It can help manage oxidative stress and support digestive health.
Aucklandiae Radix
The herb Mu Xiang in Chorus is known to affect bile. It promotes bile secretion and improves gallbladder function and oil digestion.

About the Author
Brehan Crawford, based in McMinnville, Oregon, is a distinguished clinician specializing in the treatment of chronic conditions, particularly Lyme Disease and its coinfections. After earning his Master’s degree in Acupuncture and Oriental Medicine from the Oregon College of Oriental Medicine in 2009, he deepened his expertise with a 5-year residency under the mentorship of the renowned Dr. Heiner Fruehauf at the Hai Shan Clinic. A Diplomate of Oriental Medicine from the NCCAOM, Brehan has pioneered innovative methods using Traditional Chinese Medicine for chronic infections. Known for mentoring other professionals, he regularly imparts knowledge on advanced Chinese herbal medicine applications. Beyond his clinical pursuits, Brehan enjoys singing, cooking, and hiking.


































Recent Comments