
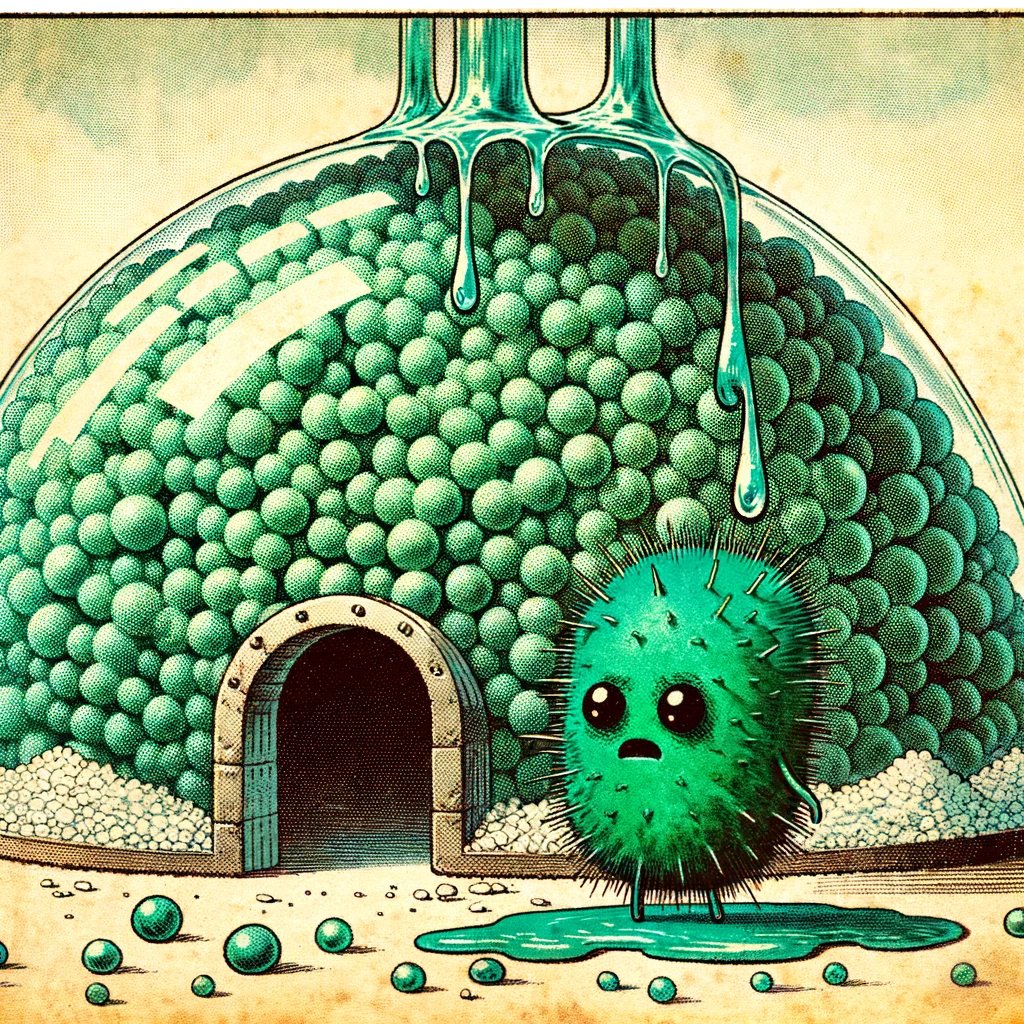
Have you ever wondered, “What is biofilm?” and why it’s a barrier to fixing your gut problems? Biofilm is a complex mucus layer that microorganisms make and hide in. It makes them harder to treat and more antibiotic-resistant.
What is Biofilm
Biofilms are complex structures formed by microorganisms like bacteria and fungi, They profoundly impact our internal environments, particularly our gut health.
A biofilm is essentially a community of these microorganisms adhering to surfaces. They produce a slimy, glue-like substance known as extracellular polymeric substance (EPS), which aids in their attachment and forms a protective matrix, altering their growth patterns and genetic expressions.
They can be found in various organs and tissues, including crucial areas like the gastrointestinal tract. Comprising up to 97% water, these biofilms create an absorbent and porous structure within our bodies, allowing the distribution of nutrients, oxygen, and microorganisms. This distribution plays a vital protecting bacteria and making them resistant to treatment.
Microorganisms within biofilms show a remarkable resistance to antibiotics, often a hundred times more than their free-floating counterparts. This resistance poses a significant challenge in treating chronic conditions and infections, particularly in the gut, where a balanced microbiome is crucial for overall health.
Quick Links to the Sections Below
How To Prevent Biofilm
Biofilms play a significant role in gut health and various chronic conditions. Understanding the factors influencing biofilm formation is crucial in managing their impact.
How Water Affects Biofilm
Water plays a pivotal role in the formation and development of biofilms. Water accounts for up to 97% of the matrix in these complex microbial structures, making its circulation crucial in biofilm regulation. Environmental factors like water flow and current significantly influence biofilm dynamics. For instance, high shear forces in turbulent flow lead to thin but dense biofilms forming, whereas laminar flow conditions result in thicker, less dense structures. These hydrodynamic conditions also affect the biofilm’s protein expression, impacting its development and stability.
Tips
- Gentle physical movement is key in influencing water dynamics within the body. It helps create vacuum forces that move water through lymphatic ducts and interstitial spaces, potentially reducing biofilm formation. Regular movement promotes sweating, an essential process for water regulation and internal cleanliness. Additionally, effective breathing acts as a natural pump, not just for air but also for water circulation.
- Maintaining proper hydration is crucial, yet it goes beyond adhering to the standard “8 cups a day” rule. Paying attention to the body’s thirst cues is vital for managing hydration levels optimally. Regular bowel movements, urination, and, for some, a normal menstrual cycle are also essential for healthy water metabolism and indirectly influence biofilm formation.
How Nutrients Affect Biofilm
Nutrient availability, especially elevated glucose levels in conditions like diabetes, fosters biofilm growth. Hyperglycemia provides an abundant source of nutrients for microorganisms, facilitating their proliferation and persistence.
Tips
- Regulating glucose levels through dietary choices, including herbs like Cinnamon and Berberine, can help control biofilm formation.
How Ions Affect Biofilm
The concentration of cations or ions with a positive charge in the environment affects how bacteria adhere to surfaces. An increase in several cations (sodium, calcium, lanthanum, ferric iron) improves the attachment of bacteria by reducing the repulsive forces between the negatively charged bacterial cells and the surfaces they attach to.
Tips
- Get Outdoors: Spend time in nature. Areas with high concentrations of negative ions, are mountains, waterfalls, beaches, parks, and forests, especially pine forests
- Balanced diet, adequate hydration, and low sodium intake, coupled with eating fruits and vegetables, can help maintain a healthy ionic balance, potentially inhibiting biofilm growth.
How Temperature Affects Biofilm
Temperature changes can significantly influence biofilm growth. Specifically, higher temperatures accelerate biofilm formation, leading to thicker and more robust structures. This is partly due to the temperature’s effect on the production of extracellular polymeric substances, which enhance the adherence of bacterial cells, a critical factor in biofilm development.
Tips
- While the human body maintains a relatively stable core temperature, micro fluctuations in local body temperatures can occur, particularly in areas with poor blood microcirculation or inflammation. These small temperature variations can create environments conducive to biofilm formation.
- Doing gentle exercise and activities promoting sweating can help improve blood circulation. This helps to maintain an even temperature throughout the body, potentially mitigating the conditions that favor biofilm formation.
How PH Levels Affect Biofilm
Biofilms flourish in base environments, specifically those with pH levels between 7.5 and 8.5. In contrast, acidic conditions with lower pH values generally lead to a decrease in biofilm production. This variation in pH influences the attachment and growth of microorganisms, directly impacting biofilms’ formation and structure.
Tips
- It’s important to note that the human body tightly regulates blood pH, maintaining a constant balanced environment.
- However, one practical application of this knowledge is the topical use of Apple Cider Vinegar, especially in diabetic wound healing. The acidic nature of Apple Cider Vinegar helps break down biofilm, making it an effective remedy for stubborn wounds where biofilms hinder the healing process.
Community in Biofilm

The composition of the microbial community plays a crucial role in the formation and functionality of biofilms. The diverse mix of microorganisms, including bacteria, fungi, and viruses, significantly influences the structure and behavior of these biofilms. and structure.
Tips
- Viruses within a biofilm can enhance their infectious capacity. Their interaction within the biofilm can turn it into a storage for viruses, maintaining their infectious nature both within hosts and in the environment. Such dynamics are vital in understanding biofilms, as they can become key reservoirs for chronic infections.
Biofilm Busting Herbs in Chorus

Citrus Peel

Citrus Peel is rich in the powerful flavonoid rutin, which can dismantle biofilm’s protective layers.
Cang Zhu

Potent volatile oils that can pass through Bioflim to kill bacteria. At the same time, it helps to balance your blood sugar.
At Home Herbs to Fight Bioflim
Understanding the factors influencing biofilm formation is key to managing their impact on gut health and chronic conditions. Implementing simple lifestyle and dietary changes can make a significant difference in controlling these complex microbial communities.
About the Author
Brehan Crawford, based in McMinnville, Oregon, is a distinguished clinician specializing in the treatment of chronic conditions, particularly Lyme Disease and its coinfections. After earning his Master’s degree in Acupuncture and Oriental Medicine from the Oregon College of Oriental Medicine in 2009, he deepened his expertise with a 5-year residency under the mentorship of the renowned Dr. Heiner Fruehauf at the Hai Shan Clinic. A Diplomate of Oriental Medicine from the NCCAOM, Brehan has pioneered innovative methods using Traditional Chinese Medicine for chronic infections. Known for mentoring other professionals, he regularly imparts knowledge on advanced Chinese herbal medicine applications. Beyond his clinical pursuits, Brehan enjoys singing, cooking, and hiking.











Recent Comments